Design and implementation of personalized T-cell therapies for solid tumors using an engineering technique to engineer a person’s T cells for their own tumors
The researchers began by separating T cells from the blood of 16 patients with solid tumors, including colon, breast, or lung cancer. T cells are part of the immune system. Each patient had dozens of receptors capable of binding to their own tumors. The team chose up to three receptors for each patient, and using Crispr, added the genes for these receptors to the person’s T cells in the lab.
“What we’re trying to do is really harness every patient’s tumor-specific mutations,” says Stefanie Mandl, chief scientific officer at Pact Pharma and an author on the study. The company worked with experts from the University of California, Los Angeles, the California Institute of Technology, and the nonprofit Institute for Systems Biology in Seattle to design the personalized therapies.
Although the efficacy of the treatment was low, the researchers used relatively small doses of T cells to establish the safety of the approach, says Ribas. He says that they need to hit it stronger the next time.
Mandl suspects the response to the therapy was limited because the patients’ cancers were already very advanced by the time they enrolled in the trial. The team decided on a few of the genes that could find the tumors, but didn’t have great results.
Bruce Levine says the ability to quickly identify patients with unique cancer genes and generate tailored treatments is very impressive. Picking the right ones that kill cancer cells will be a challenge. The fact that you can get the T cells into a tumor is something else. If they don’t do anything, that’s disappointing.
Ribas and his colleagues are searching for genes that are found in the tumors but not in the blood. Each individual in the trial had their own task done. Ribas says that there are not the same things in every cancer. “And although there are some shared mutations, they are the minority.”
Joseph Fraietta, who works at the University of Pennsylvania on T-cell cancer therapies, says the manufacturing process is very complex. In some cases, the entire procedure took more than a year.
And as researchers develop ways to speed up the therapies’ development, the engineered cells will spend less time being cultured outside of the body and could be more active when they are infused. The technology will be better, says Fraietta.
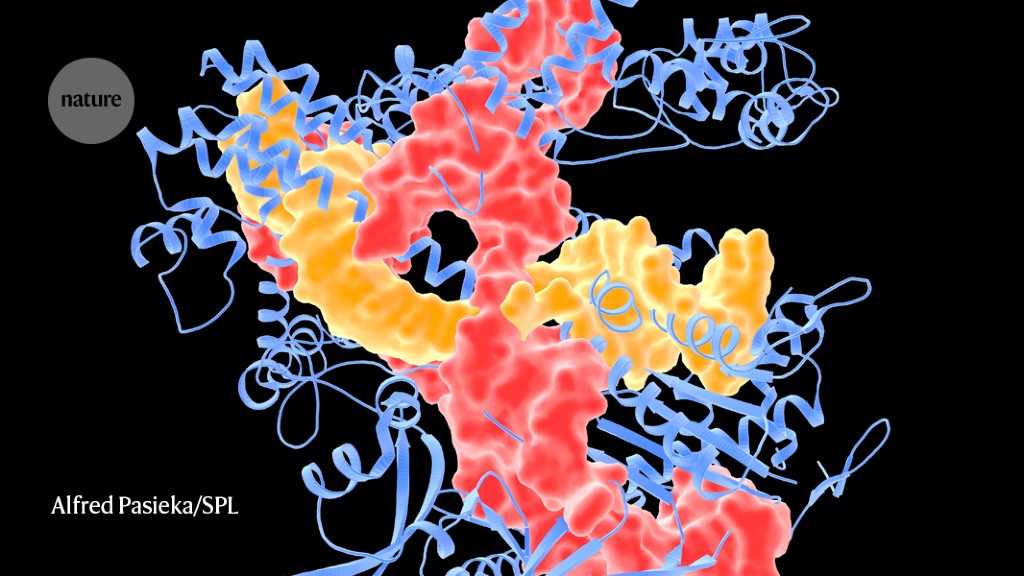
Engineered T cells — called CAR T cells — have been approved for the treatment of some blood and lymph cancers, but solid tumours have posed a particular challenge. CAR T cells are effective only against proteins that are expressed on the surface of tumour cells. It is not necessary to develop new T-cells for each person who has cancer because of the fact that the same kinds of proteins can be found across many different types of cancer.
But common surface proteins have not been found in solid tumours, says Fraietta. And solid tumours provide physical barriers to T cells, which must circulate through the blood, travel to the tumour and then infiltrate it to kill the cancer cells. Tumour cells also sometimes suppress immune responses, both by releasing immune-suppressing chemical signals and by using up the local supply of nutrients to fuel their rapid growth.