The placebo effect and observer bias on the MDS-UPDRS open label trial of regenerative therapies for the treatment of Parkinson’s disease
Our results demonstrated a beneficial effect on MDS-UPDRS part III during both on- and off-time periods. During off-time, the improvements were 32.4%, 45.1% and 50.0% for PD03, PD06, and PD07, respectively. Considering the increase in 18F-DOPA uptake, these results suggest that grafted cells function as DA neurons, therefore functionally replacing lost DA neurons. The placebo effect and observer bias may be an influence on the results of the open label trial. An analysis of placebo responses in 9 double-blind, randomized trials of regenerative therapies for the treatment of Parkinson’s disease reported an improvement of 4.3 points on the MDS-UPDRS part IIIOFF score. Moreover, a PET study conducted in four out of nine trials showed no significant increase in 18F-DOPA uptake in sham-operated groups. Furthermore, the placebo effect in patients with PD is thought to be mediated by the release, rather than synthesis, of endogenous DA in the striatum35. The three patients who exhibited motor symptom improvements exceeding what could be attributed to placebo responses, were all from this trial and may have been caused by the graft. This interpretation should be further validated through post-mortem histological examinations in the future.
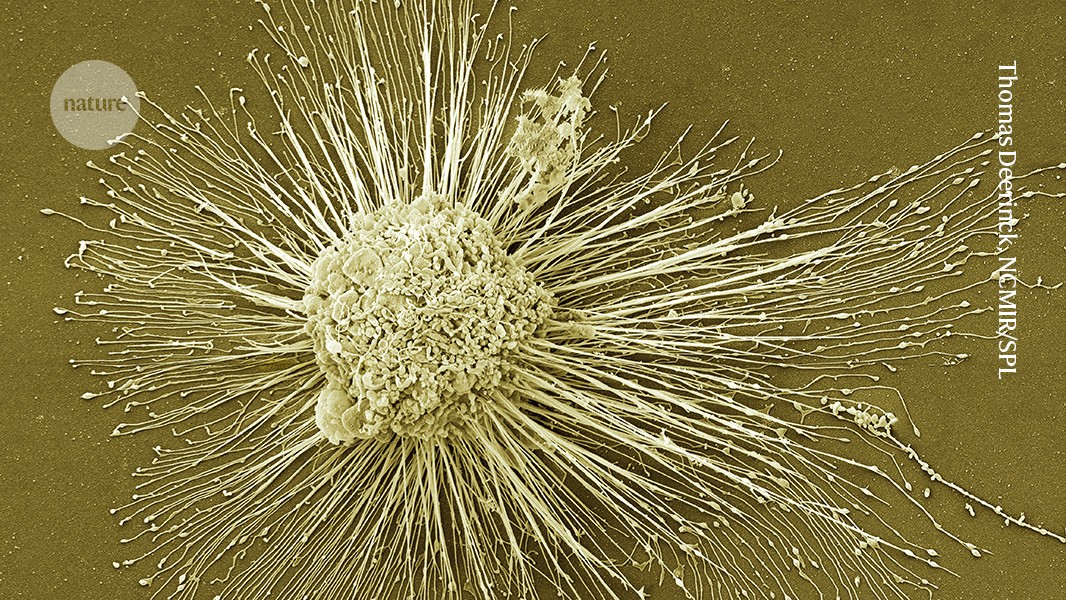
In March of this year, results were published suggesting that the cells survived and were safe one year after surgery for three individuals. The signs of benefit are not unanimous. One of the three individuals said she could see her husband’s face clearly for the first time in ten years, but only through a small section of her eye, where the cells had been transplanted.
A trial to evaluate the efficacy of a stem-cell transplant technique for Parkinson’s disease in the 2021-2021 phenomenological year
The trials were mainly designed to test safety and were small, involving 19 individuals in total, which is not enough to indicate whether the intervention is effective, says Parmar.
The small number of cells that were transplanted in the first stages of the trials might explain why some people got better and others didn’t.
The results are welcome news for a large number of people. In the year 2021, some 11.8 million people were living with Parkinson’s, double the number from 25 years earlier. According to a study published by The BMJ 4, the numbers could be 25 million in the next quarter of a century.
The stem cells were injected to 18 sites across the putamen in both hemispheres — “to roughly fill up that region of the brain”, says Viviane Tabar, a neurosurgeon at the Memorial Sloan Kettering Cancer Center in New York City who conducted the US surgeries.
In order to have 100,000 and 300,000 cells survive the surgery, five individuals received a dose of 0.7 million cells and seven received a dose of 2.7 million cells. A good brain usually has 300,000 dopamine- producing neurons. The recipients were given immune-suppressing drugs for one year after the surgery to prevent their bodies from rejecting the transplant.
Brain scans show an increase in dopamine production, which may suggest that the participants did not stop receiving drugs during the 18 month observation period.
Individuals who received the low dose showed a 9 point improvement in their symptoms, while those who received the high dose showed a 23 point improvement. The assessment measures individuals’ daily life activities, pain levels, sleep and eating. Agnete Kirkeby, a stem-cell scientist in the University of Copenhagen is involved in a European trial and believes that this metric is subjective and can be swayed by the placebo effect.
Effects of pluripotent stem cell grafts on motor impairment in PD05 and PD06: A Japanese pediatric neurosurgeon’s trial
Yamanaka, who runs a lab at Kyoto University, discovered in 2006 that adult cells could be reprogrammed into an embryonic-like state, capable of becoming practically any kind of tissue1. These induced pluripotent stem cells — or iPS cells — won Yamanaka the Nobel Prize in Physiology or Medicine in 2012, and propelled him to superstar status. They have become a symbol of the country’s global scientific aspirations.
Three people received up to five million cells, and four others received up to 11 million cells, with 150,000 and 300,000 cells expected to survive. “This low survival rate is a big problem that needs to be solved,” says Jun Takahashi, a neurosurgeon at Kyoto University in Japan, who led the trial. They were given immune-suppressing drugs for 15 months.
The off-time period improved for only one of the patients who exhibited an effect on the part III. The evaluations are based on the patient’s perception. It is possible that patients had such high expectations for the new treatment that results did not meet them. In the remaining two patients (PD05 and PD06), motor deficits stabilized at a similar level of decline to those receiving conventional medication36,37. These two patients exhibited a higher degree of deterioration in motor symptoms compared with the other patients during the on-time, suggesting that faster neurodegeneration, especially in the non-dopaminergic systems, diminished the beneficial effects produced by the graft during the trial period. Recent research shows that younger patients with less severe symptoms appear to be more appropriate for this treatment than those who are 69 years old. Considering these results, refining patient eligibility criteria may enhance the efficacy of this treatment.
The Hoehn–Yahr stage had some discrepancies between the part III scores and those of the MDS-UPDRS. The Hoehn–Yahr stage emphasizes mobility issues, whereas the MDS-UPDRS part III offers a more comprehensive evaluation of major motor symptoms. Consequently, improved postural stability and mobility may account for the greater improvement in the Hoehn–Yahr stage compared with changes observed in MDS-UPDRS part III scores of this study.
Autologous Retinal Cell Therapy: A Way to Prevent and Prevent Vision Loss in a Scientifically-Disordered World
Japan is brimming with signs of an approaching medical revolution. Shiny white robots are tending dishes of cells, rows of incubators hum in new facilities, and a deluxe, plush-carpeted hospital is getting ready to welcome its first patients.
It is important that policymakers and the public know why careful and thorough evaluation of new science-based medical products is best for patients, researchers and organizations. Researchers have been working on regenerating medicine for decades, and have made it to the point of clinical application. Regulators around the world must not put that promise at risk by rushing the final stage of the process.
The public is hesitant to try this treatment because of the high costs, large trials that show clear clinical benefit, and concerns about safety. We need to figure out what the potential of these cells are and what the limits are.
Yamanaka promised to circumvent a bioethical stand-off that had threatened the potential of embryonic stem cells. iPS cells were considered less fraught because they don’t require the destruction of human embryos. They promised to give transplantable tissues without the use of immunosuppressive drugs, as long as they could be made from the cells of the person in need.
In 2014, Takahashi put this idea to the test. She took skin cells from a 70-year-old woman with a progressive eye condition known as macular degeneration and guided them into a younger, more pliable state using a recipe similar to the one Yamanaka had devised and refined. The resulting iPS cells were then grown into thin sheets of retinal cells and transplanted into the woman’s eye, where they have survived for ten years and prevented further vision loss, Takahashi says.
It was a procedure that did not fit in with reality. Self-derived, or ‘autologous’, cell therapies are time-consuming and expensive to make, and the large cell-sheets that researchers crafted for implantation required intrusive surgery. Takahashi says she chose this approach to ensure the highest chance of clinical benefit — to demonstrate to the world what was possible. It was designed to be “scientifically, the best treatment”.
The difficulties might come down to the retina’s natural resistance to regeneration. But other parts of the eye might benefit more from cell therapies: the cornea, the clear covering that lets light in, is maintained by a pool of stem cells and constantly being rebuilt.
A journey of life and work in Japan to develop iPS cells and treatments for stroke. A review by N.J. Nishida
Nishida has since set up a start-up company, Raymei, which plans to launch a larger trial and aims to gain formal approval in three years. “The next clinical trial is pivotal,” he says.
The regeneration of nerve tissue has been one of the great hopes for iPS cells, but it has faced challenges. Jun is the husband to Masayo and he has an office full of statues of elephants and samurai armour to encourage his lab.
But, unlike his wife, he has not set up a company to develop the technology for manufacturing the cells and conducting the surgery. He transferred that knowledge to the company based in Osaka. “As a scientist, I am kind of satisfied,” he says. He has focused his attention on developing cell therapies for stroke.
Some researchers have raised concerns about this fast-track process and related programmes in Japan. Last year, two of the four products that had received conditional approval under this mechanism — one involving thigh-muscle cell transplants for the heart, the other a gene therapy to treat ulcers in narrowed arteries in the limbs — were withdrawn. The first was rejected for formal approval after nearly a decade on the market because it failed to show clinical benefit. The second was withdrawn because of a lack of results from earlier trials.
Companies can offer the treatments, with costs mostly covered by the national health system. They need to continue collecting data to get full clinical approval.
Companies that roll out interventions as quickly as possible are more likely to get a product approval in the future. This has led some to call for the efficacy requirements for conditional approval to be raised.
Masayo Takahashi’s machine learning-powered portable robotic manufacturing model: A comparison of four-week early-stage clinical trials
A white and muscular-looking two-armed robot was chosen as Masayo Takahashi’s portable manufacturing model. Powered by machine learning, it checks in on cells’ progress as they are prepared for transplant through a microscope. In 4 months, it can produce enough cells for more than 800 individual treatments.
The work can transform lives but it’s important that the work doesn’t move fast in the clinic. Researchers should be allowed to complete safety and efficacy tests in a reasonable amount of time.
The results of the early-stage clinical trials show that the interventions were safe and that the recipients of the interventions experienced some improvements in their symptoms.